BLUESTONE LAB, UCSF
The Bluestone lab is broadly focused on understanding mechanisms regulating T cell activation. Our work has centered on altering cell signaling
T cell phenotype and functional variations in patients with Type 1 diabetes.
For this project we looked at the differences between patients who retain beta cell function and still produce clinically significant amounts c-peptide-an indicator of insulin production and those who do not. Our hope is to find biological markers that could indicate whether a patient would benefit from certain therapies like immunotherapy.
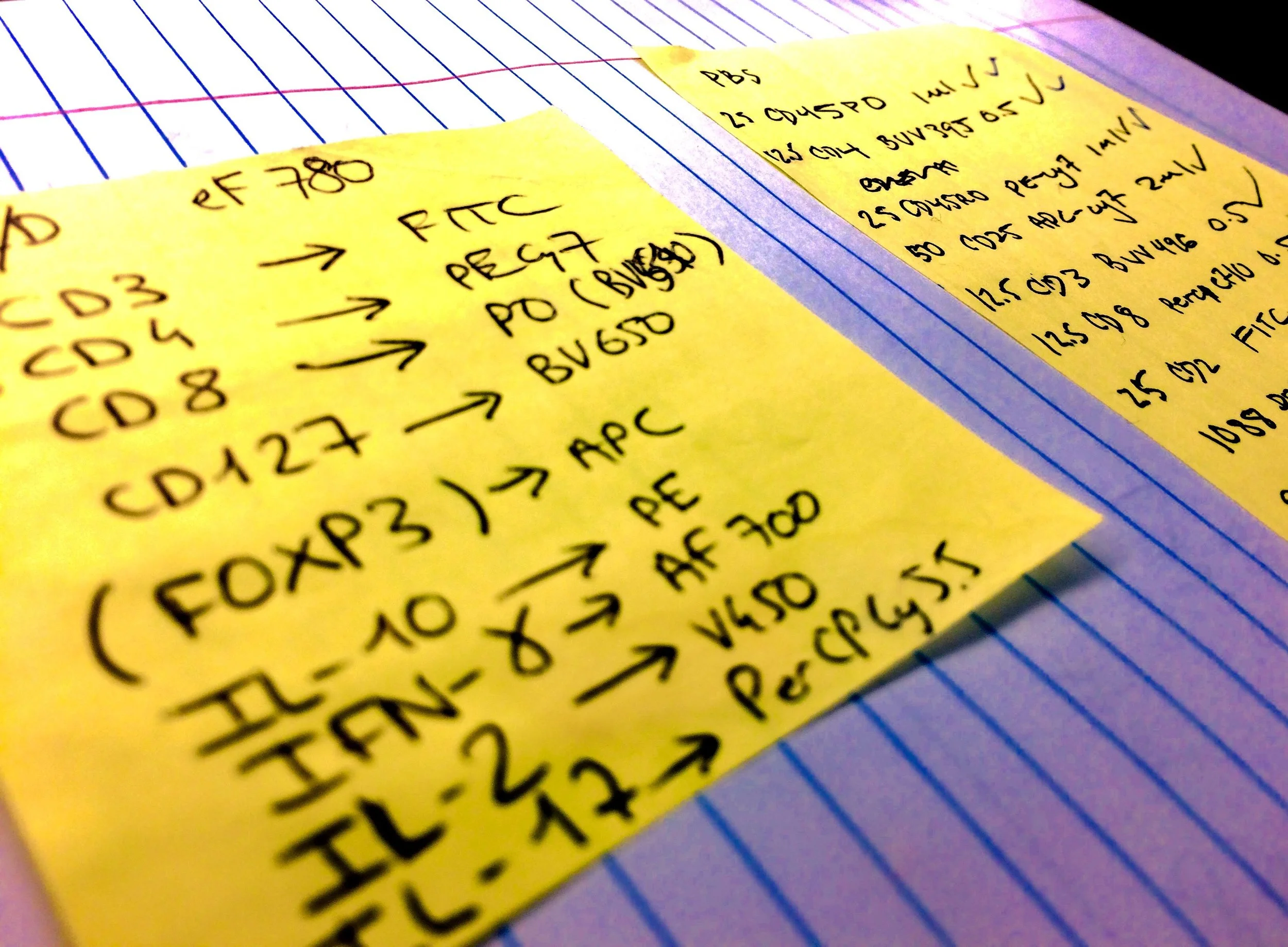
We are also interested in the T helper populations differences between Type 1 diabetic patients who retain beta cell function and those who do not. To examine this we are defining T helper populations using guidelines outlined by immunologists such as Federica Sallusto, Dan Campbell, and Thomas Duhen. Since type 1 diabetes is a Th1 mediated disease is is imperative to look at this population in comparison to Th2 and Th17 subsets. In this study we are interested to see if there is Thelper subset population variation between patients who retain beta cell function and those who do not. The Th17 cell subset is a fairly newly discovered cellular population that specializes in mediating mucosal immunity. This interesting subset has been shown to have a plastic phenotype in that they can fain a Th1 phenotype under certain conditions in mouse models. So, we are particularly interested in looking at the differences in Th17 populations in patients who have unique diabetes clinical profile
I also participated in conducting T cell functional assays for an IPEX (immunodysregulation polyendocrinopathy) patient. Typically patients with IPEX do not live past the first 2 years of life. I am assisting in the comparison of this patient's Tregs and Teffectors in functional assays to healthy donors. The most exciting part of this in my opinion is that we can incubate these cells with potential molecules in the functional assay to manipulate the patient's cells to behave as a healthy person's.
Immunosuppressant Pharmaceuticals
I also participated in a project aimed at elucidating the mechanism of action of various modifications of LFA3-Fc molecules. This is in collaboration with industry to improve an immunosuppressant drug that has proven to be effective in clinical trials for psoriasis and T1D. This has been an exciting project for me because I have been able to gain insight into industrial biology and drug development, not to mention it is an exciting opportunity to discover how a these works with the immune system which is not currently known. I have also been lucky to be able to learn how to work with humanized NSG (NOD-scid gamma mice) in order to test LFA3-Fc molecule variants in in vivo conditions. I am very excited to participate in research that could be used to help people in the near future. This is exactly the reason I love translational biomedical research!
Engineering T-Reg Receptors to Suppress Autoimmunity in Rheumatoid Arthritis
Our goal for this project is to engineer Tregs with CAR (Chimeric Antigen Receptors). The objective is to create Tregs with receptors specific to a protein that is present in the sinovial tissues of patients with RA. These Tregs would then be able to suppress autoimmune reaction from Tcells that destroy joints. Several studies have recently been published linking microbiota populations to drug therapy effectiveness in Rheumatoid Arthritis. It would be incredibly exciting to use microbiome data from a patient to screen for who might need immunotherapy instead or in conjunction with pharmaceutical treatment.